Hello! This is likhita. M
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians singned informed consent. Here we discuss our individual patients problems with an aim to solve the patient’s clinical problem with collective current best evident based input.
This E blog also reflects my patient cantered online learning portfolio and your valuable inputs on the comment box is well.
July 30 2023
This is the case of a 60 year old male , daily wage worker by occupation , resident of Rajanna gudam who presented to the hospital with
Chief complaints of
- Tingling sensation in lower limbs since 1 yr
- pain in the abdomen since 2 months
- increased frquency of urination since 1 month
History of presenting illness
- The patient was apparently asymptomatic 5 years ago when he had a fall from the lorry and sustained an injury to his back. He then notice that there was a gradual loss of strength in his right leg and had difficulty in walking. Only limited movements could be done. Gradually strength in his leg started returning and can walk with the support of a stick now
- 3 years back he was diagnosed with Diabetes in miryalguda hospital in a regular check up and was put on medication (metformin tablets)
- 1 and a half year back He apparently noticed some blisters on his left palm and bursted them whenever he saw them. Then he one day saw that they weren't healing and neglected them which lead to necrosis of his middle finger.
- He then started having tingling sensation and numbness in his lower limbs 1 year ago
- He then had pain in his upper abdomen 2 months ago which was diffuse and non radiating.
It had no aggravating or relieving factors
- He also had increased frequency of urination a month ago (10-11 times a day __ 6-7 times in the night) accompanied with burning sensation which apparently reduced a while ago (3 days back)
Past history
K/c/o dm
N/k/c/o h/t ,tb , epilepsy ,asthma
No significant Family history.
Personal history
Mixed diet
Normal appetite
Sleep is adequate
GENERAL EXAMINATION
I have taken Prior consent of the patient
patient was examined in a well lit room.
Patient was conscious, coherent and cooperative.
No icterus
No clubbing
No cyanosis.
No generalised lymphadenopathy and bipedal edema.
VITALS:
Temperature- 98.6F
BP-120/80 mmhg
PR- 88bpm
RR-18cpm
Spo2-98%
SYSTEMIC EXAMINATION:
CVS-
S1 S2 heard
no murmurs heard.
R/s - bilateral expansion of chest and air entry.
CNS examination:
Sensory system: normal
Motor system:
Right Left
Tone - UL Normal Normal
LL Normal Normal
Patient felt slight pain while flexing his right knee
Power- UL 5/5 5/5
LL 3/5 4/5
Reflexes Right left
Biceps +2 +2
Triceps +2 +2
Supinator +2 +2
Knee +1 +1
Ankle 0 0
Lower limb reflexes are absent
-involuntary movements are absent
Cranial nerves
Normal on examination
CEREBELLUM
Finger to nose test normal
heel to shin test normal
GAIT
High stepping gait
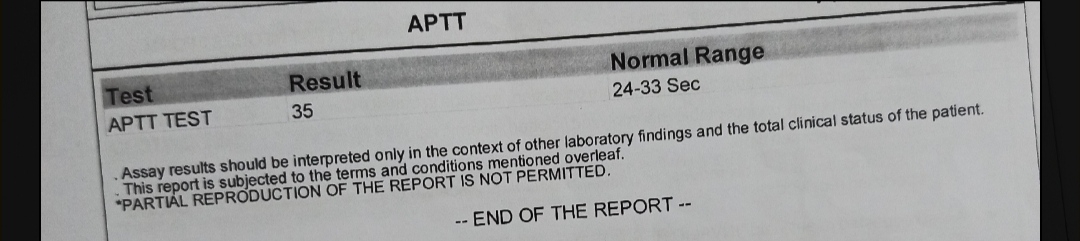
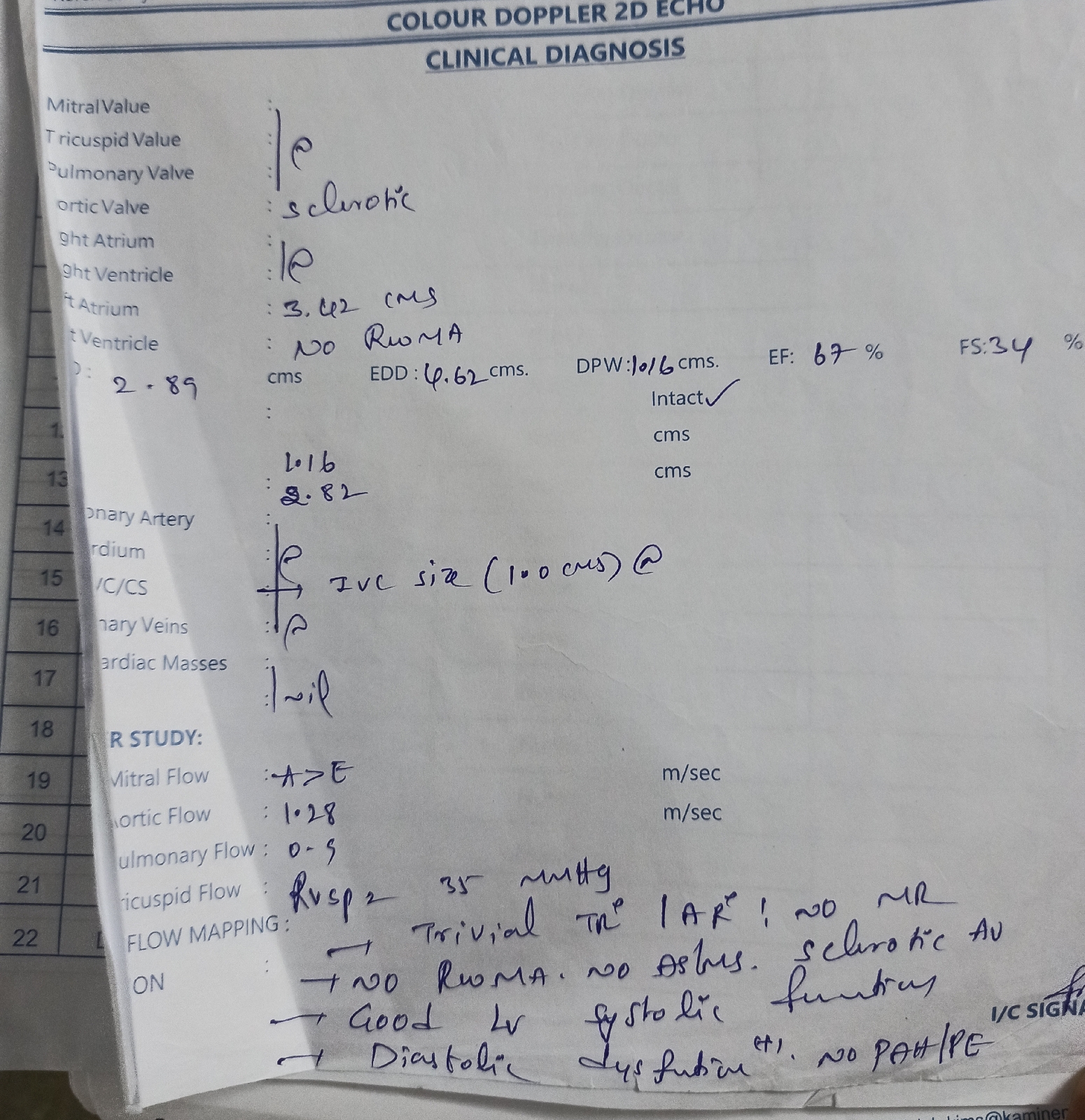
INVESTIGATIONS












Comments
Post a Comment